Dissection of the Aorta: A Rare Heart Condition Observed in COVID-19 Injected Patients
An excerpt from Taylor Hudak’s interview with Prof. Arne Burkhardt
(Watch the full interview here)
Vaccine particles appear in the bloodstream so it is not surprising that the particles are taken up by the cells of the blood vessel walls. These cells then express the spike protein and come under attack by the immune system.
Damaged cells are stripped off and expose the deeper layers of the blood vessel wall. These exposed surfaces activate the aggregation of blood platelets and the formation of blood clots.
This accounts for the numerous reports of heart attack, stroke and thrombosis after vaccination. The stability of the blood vessels themselves is also compromised. The aorta, the body's largest blood vessel, seems to be particularly affected.
Aortic Dissection
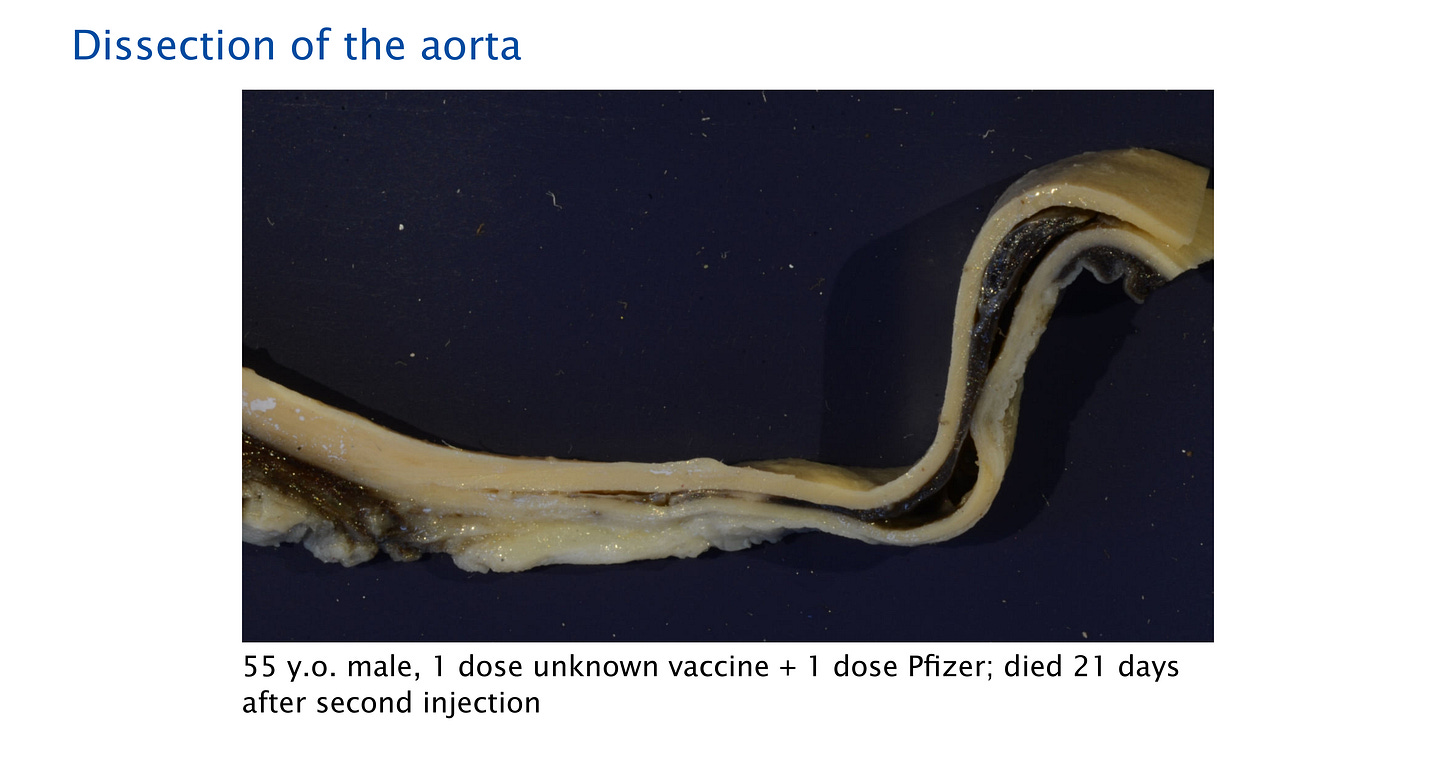
This above image shows a dissection of the aorta in a 55 year-old man, who died 21 days after the second injection. An aortic dissection is typically a very rare and serious condition, in which a tear in the aorta allows blood to rush into the vessel wall, causing it to split or dissect.
“On the left side, there’s a solid wall which is kind of yellow coloration - yellow is the color of the elastic fibers, by the way. Then you see a split formation in the middle and then on the right side, there are two walls.”
In the middle section, the black material, which is blood, has flowed into the cleft of the aortic wall. The media, which is the middle layer of the wall of a blood vessel, has been destroyed and the blood has entered, causing it to potentially rupture.
Additionally, Prof. Burkhardt examined this same aortic wall stained with Haematoxylin Eosin (HE) under the microscope. This methodology was not used during the initial autopsy. The image on the left is a lower power view whereas the image on the right is a higher power view.
“If you look at the left side, on top, you see the lumen of the aorta, where once the blood was flowing. Then there is the inner section of the aorta and below there’s a dissection, and then you have the outer wall. So, as I said, the wall is split into two.”
The red coloration is blood and the line of blueish, purple dots are inflammatory cells.
“On the right side, we have higher magnification, and here you can see the inner wall of the aorta, and on the right, the bleeding. And then in the interface, there is an infiltration of mostly lymphocytic cells and some macrophages are also there.”
Prof. Burkhardt states that an aortic dissection can have different causes, which can be best determined by viewing the specimen under a microscope. While a dissection of the aorta can be seen without a microscope, histopathological examination of the specimen can help determine the cause of the dissection.
One of the common causes of an aortic dissection is atherosclerosis, a disease of the arteries, which is frequently observed in the older population. A second potential cause is a genetic defect of the connective tissue, which appears in younger people.
However, a genetic defect does not present with any significant inflammatory infiltrates. Therefore, the presence of inflammatory infiltration, in this case, indicates the aortic dissection is not caused by a genetic defect.
“And we can further make this plausible because we did the immunohistochemistry for the spike protein, and it is selectively located (positive) in these areas. So this is an additional proof.”
An aortic dissection or rupture, which has been typically considered a rare condition, may become a more common diagnosis. Prior to the implementation of the COVID-19 injections, Prof. Burkhardt observed approximately one to two aortic ruptures out of 1,500-2,000 autopsies per year. In this series of 75 autopsies, he observed five aortic ruptures.